|
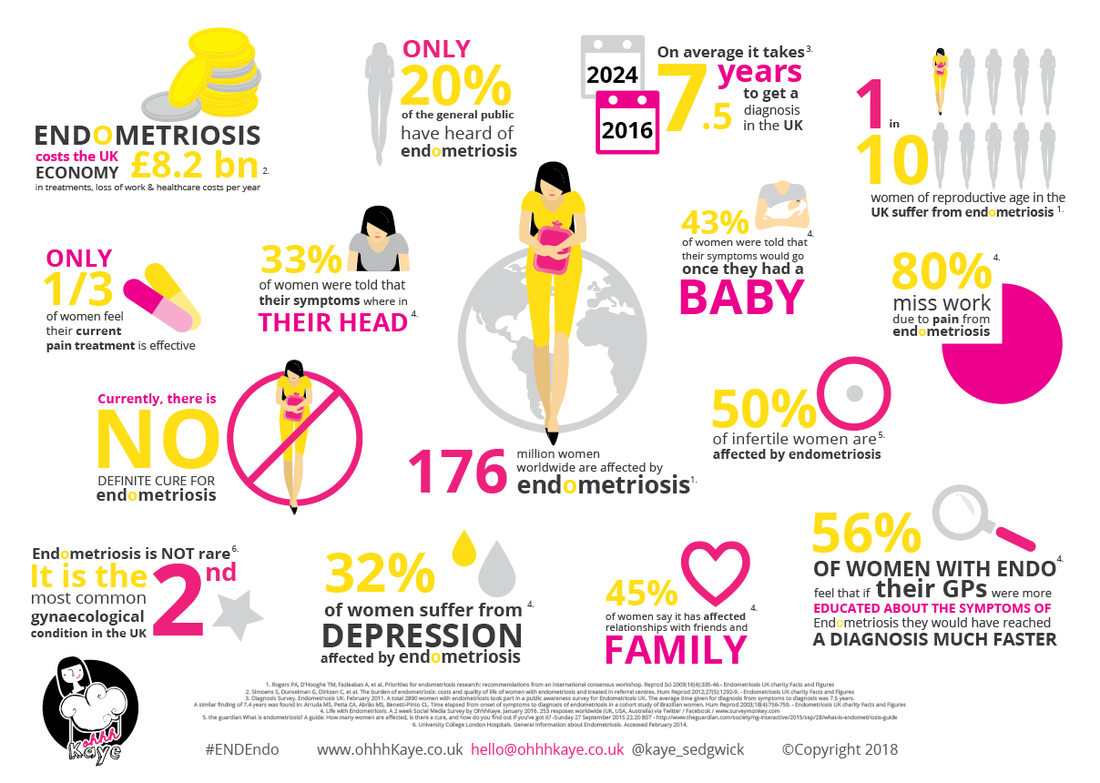
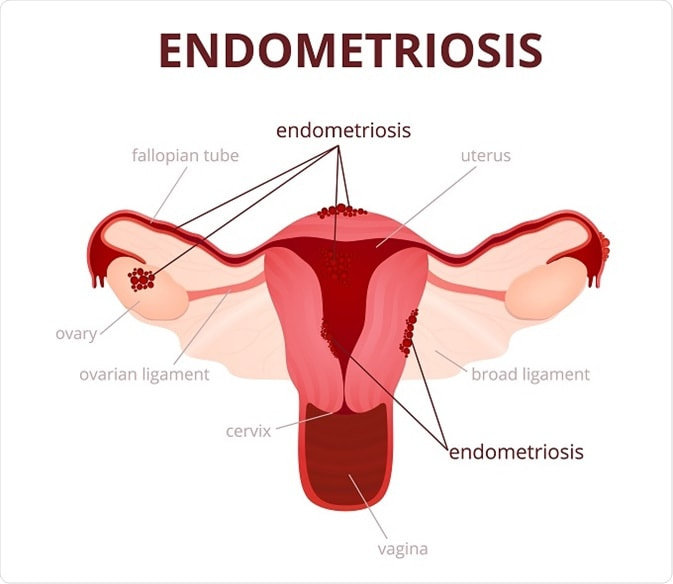
As a teenager, my periods were unbelievably heavy and incredibly painful. Feeling like someone had grabbed my lower abdomen and was twisting and wrenching it out of me. Passing clots which were like lumps of liver (apologies if you’re squeamish – I'm very open and talk about that sort of thing in my job every day!). And the flooding which happened at each bleed. Much to my dismay, I didn’t risk owning a pair of white trousers, which were quite the thing in the 80s, especially when paired with white stilettos. That was my reality every month, for several years. But thankfully, it was only for a couple of days per month. In between times I carried on life as normal. That’s not the case if you suffer from endometriosis. Crippling pain can be the norm, every day for years and years. Living with this condition is incredibly debilitating and can have a huge impact on your life - affecting your work, mental health, close relationships with partners/family, social life, sex life, and potential to conceive. March is Endometriosis Awareness Month, so hopefully this article will give you more information about the condition and different ways in which it can be managed. So what is endometriosis? Only 20% of the general public have heard of it. Here’s the science bit: the cells or tissue that form the lining of the uterus, the endometrium, normally grow inside the uterine cavity. In endometriosis it grows elsewhere, such as the ovaries, pelvic ligaments, bowel, bladder, rectum or outside the uterine cavity entirely. In women with endometriosis, the displaced endometrial tissue (also known as implants) functions and is influenced by hormones just as a normal endometrium is, and therefore can bleed during menstruation. When the uterine lining is shed during a period, the implants also bleed, except the blood becomes trapped inside the body. The accumulated blood causes localised inflammation and is painful. Over time the growth of the implants, the repeated internal bleeding and inflammation may cause the development of adhesions or scar tissue. What are the symptoms? Endometriosis sufferers can experience a range of different symptoms which vary for each person depending on where the endometriosis is and the organs affected. Symptoms can include heavy, painful periods (dysmenorrhoea) with large clots, long or irregular cycles, bleeding between periods, lower abdominal pain, back pain, or chronic pelvic pain which can last all month long, painful sexual intercourse, pain during bowel movement or urination, rectal bleeding, swollen, painful ovaries, swollen abdomen, fatigue, and fertility problems. What are the causes or risks of getting endometriosis? There are a number of causes and risk factors which may increase the chances of you getting endometriosis. The main cause is likely to be retrograde menstruation. This is when the endometrial tissue passes through the Fallopian tubes into the abdominal cavity, instead of passing out through the vagina. Women whose mother, grandmothers or sisters have endometriosis have an increased risk of getting it, as do those who have had a hysterectomy. Low progesterone disrupts hormonal imbalance overall. When progesterone is low, oestrogen usually becomes too high. Endometriosis is an oestrogen sensitive disease and symptoms are increased by oestrogen during the menstrual cycle. We are exposed to many xeno-oestrogens (meaning man-made) through foods, plastics and cosmetic products. These can increase the irritation and hormonal activity of the endometrial tissue. Symptoms are increased by inflammation. Today's western diet is highly inflammatory with an imbalance in the ratio of good to bad fats, processed foods and exposure to chemicals and hormones in non-organic foods, particularly meat and dairy. There is current research stating that endometriosis is classed as an auto-immune disease. This may explain why it tends to be hereditary, as auto-immune conditions are often passed through generations. How can it affect my fertility? Endometriosis is the second most common gynaecological condition in the UK, and up to 50% of ‘infertile’ women (presumably that means those who are trying to conceive and have been given an ‘unexplained infertility’ diagnosis) are affected by endometriosis. That’s huge. It is an oestrogen dominant condition so causes hormonal imbalance. Proper hormonal balance is essential for healthy fertility. Every month, the excess tissues bleed which cause inflammation and scar tissue, affecting the uterus, Fallopian tubes, and ovaries. This is known as chronic pelvic ‘congestion’ and may alter normal functioning of the ovaries, cause blockages in the Fallopian tubes, or make it harder for an embryo to attach properly to the wall of the uterus for implantation. Some research also suggests that the woman’s body may form antibodies against the misplaced endometrial tissue. These same antibodies may attack the uterine lining and cause miscarriages (up to three times the normal rate). What is the treatment for endometriosis? There is no cure for endometriosis. With conventional medicine, there are 3 main treatment options – surgery via laparoscopy, hormone therapy ie the pill or inducing medical menopause (which isn’t helpful if you’re trying to start a family), and pain management, usually with medication. I never did get to the bottom of what was causing me such painful, heavy bleeds as a teenager. My GP put me on the pill aged 14, and said that having a baby in due course would probably improve things greatly. Hmmm, not particularly sound advice to a 14 year old - I thought doctors were meant to be discouraging teenage pregnancies! For those with endometriosis, there are other more natural treatment options too, where the main aim is to support the proper functioning and health of the endometrium, endocrine system and immune system and allow you to live your life not limited by your condition. So what are these alternatives which may help to you to manage your symptoms? Here are our 12 top tips: 1. Reflexology My training with the Association of Reproductive Reflexologists (ARR) taught specific treatment protocols for endometriosis. The most effective time for a reflexology session is during the bleed, when lesions will be most active, so treatment can clear stagnation and debris in the system. It’s also the most useful time to manage any associated pain in the abdomen, bloating, constipation, etc. However, reflexology is also useful for balancing hormones throughout the whole menstrual cycle. In a small study carried out by the ARR, of those patients who presented with endometriosis, 65% became pregnant and 55% went on to have a live birth after having a course of reproductive reflexology treatments. Find a qualified Reproductive Reflexologist or book a reflexology treatment with me or one of my colleagues. 2. Fertility Massage This specialised treatment works on the lower back and abdomen, and can be beneficial to those with endometriosis in several ways. Oestrogen clearance takes place in the liver, therefore by increasing the circulation and strengthening the liver you are helping your liver to eliminate toxins including the excess oestrogens. Increased circulation will assist with maintaining hormonal balance. Hormones travel in our blood, therefore by clearing congestion in the pelvic region allows for a freer blood flow, thus encouraging the negative feedback loop between the ovaries and pituitary gland to function better. Scar tissue and adhesions which cause congestion are softened and reduced due to the increased circulation of blood and lymph. Increasing the circulation to the uterus will increase fresh oxygenated blood, which renews and repairs cells, so will increase uterine tone. On an energetic level, massage will release blocked pelvic energy. It also releases endorphins, which is a wonderful natural form of pain relief. Find a qualified Fertility Massage Therapist or book a massage treatment with one of my colleagues. 3. Eating the right food Dietary changes specific to endometriosis are important. There are several types of food you may want to avoid because they have been linked to making endometriosis worse. Certain foods may trigger flare-ups, promote inflammation, or are ‘congesting’ to the body, feeding the congestive nature of endometriosis, while other foods may increase hormonal imbalance. Foods to limit or avoid:
Foods to eat plentifully:
4. Bee Propolis If you’re trying to conceive, consider taking bee propolis. It’s basically a resin-like substance made by bees consisting of beeswax, saliva, sap, and various botanical products from the surrounding area. A study showed that 60% of women with endometriosis related infertility who took bee propolis for 9 months became pregnant, as opposed to 20% in the placebo group. Suggested usage is 500mg of bee propolis, twice a day. It also provides amazing immune support and people who take it regularly never get colds or other lurgy apparently! 5. NAC (N-acetyl cysteine) NAC (N-acetyl cysteine) is an amino acid. A study was designed to compare the progression of ovarian endometriomas in NAC treatment patients and untreated control patients. Patients were given either NAC 600 mg three times daily, 3 consecutive days per week or not, for an observation period of 3 months. At the end of the 3 month observation period, endometriomas (ovarian cysts or chocolate cysts related to endometriosis), were evaluated by pelvic ultrasound, by a trained physician, who was blinded as to which group the patients had been in. In the NAC treated group, 24 patients cancelled their scheduled laparoscopy due to a decrease or disappearance of cysts, pain reduction or pregnancy. In the control group, only 1 patient cancelled surgery. Also in the NAC treated group, 14 women had decreased ovarian cysts (-1.5 mm average), 8 had a complete disappearance, 21 had pain reduction and 1 became pregnant. NAC influences the development of endometriosis in various ways. It decreases multiplication of abnormal cells, decreases the invasive behaviour of the endometriosis cells, decreases inflammatory substances, regulates expression of inflammation related genes, and stimulates cell differentiation. NAC may be useful for the treatment of current endometriomas, as well as endometriosis, and potential prevention of recurrence after a surgery. However, as with all supplements, it is best to get advice from a qualified nutritionist first. 6. Herbal Medicine Herbs and supplements can be very helpful for women with endometriosis. Many of these plant based substances support the body in eliminating excess hormones, endometrial tissues, and inflammation, while promoting the reduction in endometrial growth. These herbal remedies may be beneficial in the treatment of endometriosis:
7. Castor Oil Packs Castor oil packs have been said to help detoxify the liver naturally (therefore eliminating excess hormones), support uterine and ovarian health, improve lymphatic circulation, and reduce inflammation in the abdomen. There aren’t any conclusive studies on the use of castor oil packs externally (though there are some preliminary ones), but a long history of traditional use in many cultures. You can buy a complete kit or just the castor oil and use an old towel or woollen flannel. You soak the towel or flannel in castor oil and place it over your lower abdomen/uterus or wherever you are feeling pain. Make sure to cover the liver too which is on the right of your abdomen. Then cover it with a bit of cling film or plastic bag, followed by a hot water bottle or microwaveable heat pack. I love this one filled with cherry stones – it retains heat longer than wheat-filled ones, can be washed so is more hygienic and is 25x25cm so larger than many others and covers most of the abdomen. You then have to lie still with feet elevated for at least half an hour, so it’s a bit of relaxing time out to yourself which has health benefits in its own right! Do it at least twice a week if possible. The process can be a bit messy, so make sure you lie on top of an old towel or sheet/shower curtain combo to avoid castor oil drips on your best sofa. It’s definitely worth the effort though. 8. Progesterone If you have endometriosis, Dr. John Lee recommends using progesterone cream from days 8 to 26 of your cycle, to counter balance the effects of oestrogen on the body as it stimulates endometrial growth. Take a short week off to refresh your receptor sites. He has had success with controlling symptoms within six months. Once the outbreaks of endometriosis are tolerable reduce the usage to day 12 until you get your period. 9. Yoga Yoga can help those who suffer from endometriosis in many ways – physically, emotionally and physically. Deep breathing techniques are important as they decrease stress hormones and increase the feel good hormones in your system. There are various poses which can help to stretch out the lower back, ease painful trapped wind, and increase blood circulation in the pelvis. If you’re in Edinburgh, try Penny Horner’s nurturing Well Woman Yoga classes at KnotStressed. Or have a look at Helen Kaselov’s site www.endoyoga.com 10. Avoid hormone disruptors via environmental toxins We know that exposure to certain environmental toxins (synthetic xeno-oestrogens) may contribute to the development of endometriosis or make it worse because they are endocrine disruptors. These chemicals have the ability to interfere with the natural functions and development of our bodies. The main function of the endocrine system is to serve as our body’s message centre. Hormones deliver messages, the endocrine system coordinates the hormones. Ways to support healthy endocrine function and avoid xenohormones:
11. Urinary Tract Infections UTIs and cystitis can be common if you have endometriosis, especially if you experience painful sexual intercourse. The most common way of treating UTIs is with antibiotics, however, prolonged use of antibiotics due to recurrent UTIs can have several side effects, such as antibiotic resistance, adverse physical side effects eg rashes, nausea, and diarrhoea, and eradication of the normal flora (good bacteria) in the gut. These microorganisms are essential to the healthy function of the immune system, so overuse of antibiotics can lead to poor immunity and being susceptible to other infections and illnesses. An alternative treatment to antibiotics for cystitis and UTIs is the supplement D-Mannose. It works by "sticking" to E. coli lectins preventing the adhesion of E. coli to the lining of the bladder and urinary tract thus helping to prevent replication. Bacteria is then flushed away through normal urination. D-Mannose does not interfere with blood sugar regulation because it is non-glycaemic in humans. It’s definitely worth a try if you suffer from recurring UTIs. 12. Get support
If you have endometriosis, you don’t have to suffer alone. There are some fantastic resources available to support you. Endometriosis UK is the largest endometriosis charity in Britain so have a good look at their website as it's full of great information. They also run local support groups in towns and cities all over the UK, including Edinburgh. Endo Sister Kaye Sedgwick Jones is a graphic designer and illustrator who has produced a wonderful e-book called Living With Endometriosis, kindly available to download for free. Other sites with some fab resources and articles are thisendolife.com and endometriosisnews.com And just by using the hashtag endo, endometriosis, endo sister or endo warrior on instagram, facebook or twitter, you’ll find loads of other amazing women living their best lives with this debilitating condition so don't be scared of opening up and finding your tribe. #endendo Comments are closed.
|
If you would like to collaborate with a guest blog, please get in touch by email. I'm interested in articles about fertility, pregnancy, parenthood, complementary therapies, book or product reviews, local practitioners or classes, and general health and well-being. My horizons are pretty broad, so if you have something you'd like to write about, please do!
Archives
September 2023
Categories
All
|
© COPYRIGHT 2024 Fertility and Pregnancy Limited








 RSS Feed
RSS Feed